A novel treatment for antibiotic resistance that impacted my journey
My name is Chris Shaffer and for 45 years I worked in public education in Ohio and California, USA. I was a music and special education teacher early in my career before becoming a high school principal and district leader. Toward the end of my career, I moved back into the classroom for 6 years and served as a special education classroom teacher one more time before retiring.
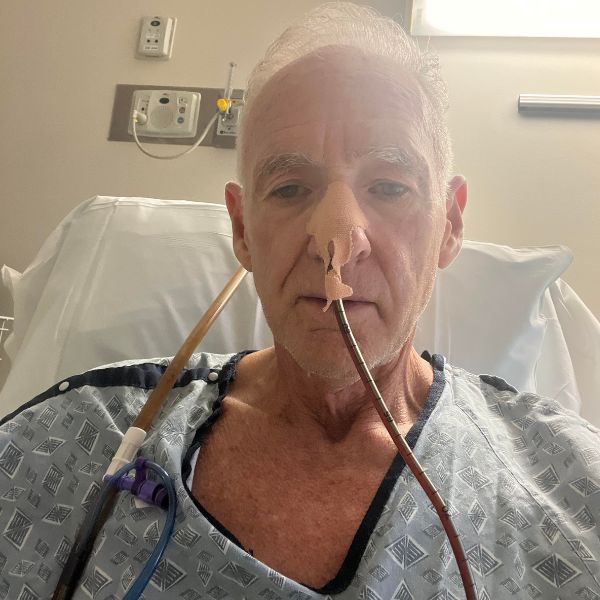
In April of 2021, after enduring three abdominal surgeries and several emergency hospitalisations for blocked intestines related to diverticulitis, I found myself with a life-threatening infection.
E-coli with extended-spectrum beta-lactamases (ESBLs) had taken up residence in my prostate. ESBLs are resistant to many penicillin and cephalosporin antibiotics and often to other types of antibiotics.
Sure enough, the bacteria in my body were not responding to any antibiotics. It was a desperate situation. For two years I underwent various antibiotic treatments with the duration of each treatment extending by weeks and months.
Each time I finished a round of treatment, the symptoms would return sooner than the time before and eventually, the symptoms would appear and not retreat. When the last oral antibiotic failed, doctors recommended a 35-day round of highly toxic and dangerous intravenous antibiotics. I did not want to take that risk.
An alternative to antibiotics? I began my own research
I had realised that using approved antibiotics was likely to fail and I would die from this infection. I was left with nowhere to turn and no treatment options in Western medicine offered me any hope of a lasting cure, so I decided to look elsewhere. I had learned from doing my own online research that chronic infections are usually accompanied by biofilms. Biofilms are a thick gelatinase goo that protects bacteria from antimicrobial assaults, including antibiotics. This makes the antibiotics ineffective.
My research led me to a treatment called Phage Therapy, which is mostly found in Tbilisi, Georgia and which has existed for 100 years. Phage Therapy consists of live, friendly viruses that attack and destroy bacteria and biofilms.
I found out that for every bacterium, there is a phage virus that targets that bacterium uniquely. Once inside the body, the phage attaches itself to bacterial cells and injects its DNA into them. The phage hijacks the bacteria reproduction process, and the bacteria then create more phages, not more bacteria. Once enough new phages inhabit the bacteria, they release an enzyme which breaks open the cell wall destroying the bacteria in the process. The new phage goes on to destroy more bacterial cells until the infection is eradicated usually with no known side effects.

Exploring the reality of being cured. Could it be true?
Knowing the science behind Phage Therapy was not enough to convince me to pursue it, I needed to find someone who had experienced it and been cured. I found out about a man named Pranav Johri who had undergone Phage Therapy treatment at a Center in Tbilisi, Georgia about eight years ago and who was indeed cured.
Following his recovery, Pranav became a Phage Therapy advocate like me in his home country of India. I reached out to him and we began to talk. After my conversations with him I developed the trust in Phage Therapy that I needed to move forward.
I contacted the Phage Therapy Center, and they walked me through the process. First, I sent body fluid samples for diagnostic testing to confirm whether Phage Therapy could be an option for my infection. The response was positive, but the center said that my infection was particularly difficult and would require a custom phage preparation. This would take ten to twelve weeks.
Starting Phage Therapy Treatment
In early June 2023, the center told me my Phage treatment was ready. Five days later I boarded a plane to Tblisi and started my treatment on 9 June. I stayed for 30 days for the first round of treatment and brought the remaining medication back to the United States upon my return. The treatment was a small vial of phage liquid I drank twice a day on an empty stomach and one suppository at night. I did 3 lots of 20-day rounds with 10-day breaks between each round.
At the end of the treatment, my lab tests indicated that I was free of infection. Two years on, I remain that way.
I feel great again and I cherish every day thanks to Phage Therapy and the experts at the treatment center who gave me a second chance to live a full and healthy life.
I have now chronicled my journey in a book called Finding Phage: How I Partnered with a Friendly Virus to Cure My Deadly Bacterial Superinfection. I hope to help others learn about AMR infections and the potential of Phage Therapy.
Chris Shaffer
Chris Shaffer was a music, special education teacher, and high school principal for 45 years. At the end of his educational career, he was thrust into the world of AMR infections when a number of abdominal surgeries left him with an E-coli infection which failed to respond to antibiotics. After doctors in the USA left him with little hope for a cure, diminishing health, and a bleak prognosis, he set out on his own.
Chris found success in phage therapy in Tbilisi, Georgia. With phage therapy giving Chris his life back, he has dedicated his retirement years to advocating for and helping raise awareness of phage therapy used for AMR infections. He tells the story of his phage journey in a book titled, Finding Phage: How I Partnered with a Friendly Virus to Cure My Deadly Bacterial Superinfection. His website, phagetherpyusa.com helps others learn to understand the healing power of phage therapy.
FAQ’s about Phage Therapy answered by The AMR Narrative
Imagine getting an infection that just won’t go away. You’ve tried every antibiotic available, but nothing works. The infection keeps coming back and getting stronger each time. That’s what happened to the patient whose story we’re sharing on this blog, Chris. And it’s happening to more people around the world as antibiotic resistance rises. But in this case, something remarkable happened. The patient was cured, not by antibiotics, but by a treatment that uses viruses to fight bacteria: phage therapy. Below are a few Frequently Asked Questions.
Phage therapy is a medical treatment that uses bacteriophages, which are tiny viruses that specifically infect and kill bacteria. The word “phage” comes from the Greek word phagein, meaning “to eat,” which is exactly what these viruses do: they “eat” bacteria from the inside out.
Phages are natural. They’re found everywhere, in soil, water, and even inside our bodies. Humans come into contact with phages every day without even noticing. They’re incredibly specific, usually targeting just one species or strain of bacteria, unlike antibiotics, which can kill both good and bad bacteria.
When antibiotics fail, especially in life-threatening infections caused by superbugs (bacteria resistant to multiple antibiotics), phage therapy can offer hope. The process involves identifying the exact bacteria causing the infection and then selecting phages that are known to attack those bacteria. These phages are then delivered to the patient by injection, or sometimes directly to the infected area.

Illustration of phages attacking a bacteria
Phage therapy isn’t new. It was first used in the early 20th century, even before antibiotics were discovered. But after antibiotics became widely available, phage therapy was largely forgotten, at least in Western medicine. It continued quietly in some parts of Eastern Europe and the former Soviet Union.
Now, with antibiotic resistance becoming a global health crisis, scientists and doctors are taking a fresh look at phages. There have been a number of recent success stories, like the one we’re sharing here of Chris, where phage therapy was used to save lives after all other treatments had failed.
Countries like Georgia and Poland have decades of experience with phage therapy, and modern research institutions in the US, UK, South Africa, and Australia are beginning clinical trials. Some compassionate use programs have allowed patients with untreatable infections to receive custom phage treatments.
While phage therapy is promising, it is not a one-size-fits-all solution. Phages must be matched carefully to the bacteria causing the infection, which can take time and laboratory resources. Not all infections are suitable for phage therapy, especially if the bacterial strain cannot be identified or if no effective phages are available.
Also, unlike antibiotics that can be taken easily in pill form, phage therapy is more complex. In many cases today, it is still experimental, used only when antibiotics have failed and under close medical supervision.
There are also questions we still need to answer. How do phages interact with the human immune system? How do bacteria develop resistance to phages, and can we overcome that? Can phages be safely and effectively produced at scale?
Phage therapy holds the most promise for:
- Multidrug-resistant infections, especially in hospitals.
- Chronic infections, such as those in cystic fibrosis patients or complicated wound infections.
- Cases where antibiotics are not an option, due to allergies or failure of standard treatments.
It should not be considered a first-line treatment for everyday infections that can still be treated with antibiotics. Nor should it be used without laboratory testing and medical supervision.
We urgently need more research to fully understand the potential of phage therapy. Clinical trials, regulatory frameworks, safety data, and public awareness are all still developing. More investment is needed, not just in wealthy countries, but around the world.
If phage therapy is proven effective, it must be made accessible to all who need it. This includes people in low- and middle-income countries, where antibiotic resistance is often more widespread and where access to new treatments is limited by cost.
We must ensure that phage therapy doesn’t become yet another expensive treatment only available to the privileged few. Equity and affordability must be built into the system from the start, through local manufacturing, open research, and global cooperation.
Phage therapy won’t replace antibiotics, but it may soon become a vital tool in our medical toolbox, especially as we confront the growing threat of drug-resistant infections. For patients like the one whose story we’ve shared, phages have already made the difference between life and death.
We now stand at a critical crossroads. Will we invest in this potential and ensure it’s available to everyone? Or will we allow it to become another niche cure for those who can afford it? The time to act is now.
Disclaimer: This story is shared with the permission of the individual(s) involved and is intended for educational and awareness purposes only. It does not represent medical advice and should not be used as a substitute for consultation with qualified healthcare professionals. While we encourage you to share the story in its original format, all rights are reserved by The AMR Narrative. Please do not reproduce, modify, or use any part of this story without prior written consent from The AMR Narrative. To request permission, please contact us here.








